Studies Document the Physical and Emotional Aftereffects of Abortion
[Update: This article was initially published in 2000. For the latest information about studies on the impact of abortion, see our research and news releases pages.]
Population controllers have long insisted that abortion is healthier for women than childbirth. A host of studies examining the effects of abortion, however, have proved otherwise. Women who have abortions often face increased physical and emotional problems, including substance abuse, mental disorders, impaired fertility, pregnancy loss, and breast cancer. This article will examine the various studies and what they say about the risks of abortion.
Fatal Complications
Even though most abortion-related deaths are not officially reported as such,(1) legal abortion is reported to be the fifth leading cause of maternal death in the U.S.(2) The most recent-and best documented-study on abortion-related deaths to date is a 1997 government-funded study from Finland which showed that women who abort are four times more likely to die within a year than women who give birth. By extending their scope beyond the very narrow time frame that is examined by most post-abortion studies, the researchers were able to get a better look at how abortion truly affects women’s lives. The results clearly showed that compared to women who carry to term, women who aborted in the year prior to their deaths were:
- 60 percent more likely to die of natural causes,
- 7 times more likely to commit suicide,
- 4 times more likely to have fatal accidents, and
- 14 times more likely to die from homicide.(3)
Short-Term Complications
Abortion has also been linked to a number of short and long-term physical problems. Immediate complications can include uterine perforation, infection, excessive bleeding, embolism, anesthesia complications, convulsions, hemorrhage, cervical injury, endotoxic shock, fever, vomiting, and Rh sensitization. Long-term problem include infertility, problems with future pregnancies, certain types of cancer, and lower overall general health.(4)
Infection is one of the most common abortion complications, yet many clinics do not routinely test for or treat infections.(5) This is despite the fact that even some pro-abortion advocates have admitted that abortion can cause infection. For instance, in an article on “do it yourself” abortions, Planned Parenthood of California spokesperson Michele McDevitt warned that “any time the uterine area is invaded there’s a possibility of infection.”(6) Ironically, this is coming from the same organization that insists that abortion is safe as long as a woman pays a clinic to do it.
Infection can be even more devastating if the woman fails to seek treatment or if the clinic does not test for the existence of infection prior to the abortion. One study found that women who had untreated chlamydia infections at the time of their abortions had a 72 percent risk of developing pelvic inflammatory disease compared to 8 percent of women who were treated prior to their abortions.(7) Another study found that women with a chlamydia infection who delayed seeking treatment for three or more days from the onset of symptoms were six times more likely to develop infertility problems than those who sought treatment right away.(8)
Even when women do seek treatment right away, infections can still lead to long-term damage. Younger women who have not had a previous full-term pregnancy, for example, don’t respond as well to antibiotic treatments as older women who have previously given birth to a child.(9)
When Cancer Strikes
Approximately one in eight women will have breast cancer in their life time. An estimated 43,500 women die each year from this disease, with more than 175,000 new cases of invasive breast cancer being diagnosed each year.(10)
Studies on the abortion-breast cancer link have been dismissed or ignored by the abortion industry and the secular media. But researchers have found that by interrupting the growth of cells in the woman’s breasts during the first trimester of pregnancy, abortion may increase her risk of breast cancer.
Dr. Joel Brind, a leading expert on the abortion-breast cancer link, conducted a meta-analysis of 23 published reports on breast cancer and abortion, 18 of which documented a link between abortion and breast cancer. Brind and his fellow researchers concluded that women who aborted their first pregnancies faced a 30-50 percent higher risk of breast cancer. Seven out of ten studies also showed that women who had multiple abortions had a higher risk of developing breast cancer than women who had undergone only one abortion.(11)
The Risk to Future Pregnancies
Studies indicate that for healthy women, the risks of contracting certain problems during pregnancy and delivery are actually reduced with each subsequent pregnancy. For example, hypertensive disorders like eclampsia (convulsions) and pre-eclampsia (high blood pressure with edema or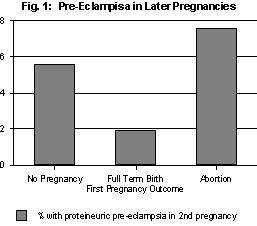 abnormal protein in the urine) are among the major causes of pregnancy-related deaths in the western world.(12)
abnormal protein in the urine) are among the major causes of pregnancy-related deaths in the western world.(12)
Research shows, however, that women whose first pregnancy ended in a full-term delivery were less likely to experience proteineuric pre-eclampsia in a subsequent pregnancy. But as shown in Figure 1, women who aborted their first pregnancy actually had an increased risk of developing proteineuric pre-eclampsia in later pregnancies.(13)
Studies have also found that women with a history of abortion have a greater risk of fetal loss than women who had previous abortions. Figure 2 shows that women with two prior pregnancies carried to term and no abortions had the lowest risk (0.71), while women with two prior abortions had the highest risk (4.31).(14)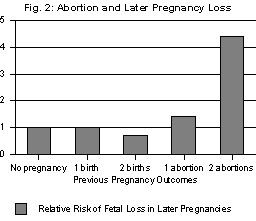
Data from other studies show that women with a history of abortion:
- Had a 1.5-1.7 times higher risk of ectopic pregnancy than women who had previously carried a pregnancy to term.(15)
- Were four times more likely to have an intrauterine infection during a subsequent pregnancy than women whose previous pregnancy had ended in a birth of at least 20 weeks gestation.(16)
- Had a higher risk of bleeding during a subsequent pregnancy than women who had previously given birth or who were experiencing their first pregnancy.(17)
- Experienced more intense pain during labor than women who had previously carried to term.(18)
- Were more likely to suffer from retained placenta during delivery or postpartum hemorrhage than women who had previously given birth.(19)
In addition, although little is known about the impact of abortion on maternal mortality rates in subsequent pregnancies, there can be little doubt that abortion increases a woman’s risk of developing a life-threatening complication during a later pregnancy. For instance, available statistics suggest that legal abortion is responsible for approximately 4800 cases of ectopic pregnancy each year. Researchers estimate that about ten women die every year from abortion-related ectopic pregnancy.(20)
Self-Destructive Behavior After Abortion
Women abort for many reasons: fear of losing a relationship, fear of disappointing their parents or partner, fear of not being able to raise a child, or fear of losing control over their lives. Often those around them send the message that if they sacrifice “just this one thing,” they can hang on to everything else in their lives.
Unfortunately, what many women don’t realize is that they end up sacrificing part of themselves as well along with their children. Abortion leaves them with feelings of self-hatred, isolation and regret. Nancyjo Mann, the founder of Women Exploited by Abortion (WEBA), wrote that after her abortion,
I began to hang around the tough crowd, imitating their ways, taking on their attitudes. What attracted me to them was their destructiveness, their contempt for the world. Soon I was carrying guns and knives, and biking around with motorcycle gangs and worse. The people I ran with were out to destroy, steal, and maim, and that is what I wanted to do both to others and myself.(21)
Such self-destructive tendencies are a common post-abortive reaction. One study found that women who had undergone abortions were treated 24 percent more often for accidents or conditions related to violence than women who had given birth.(22)
Substance abuse is another manifestation of self-destructive behavior. A recent Elliot Institute study found that women who had abortions were five times more likely to abuse drugs or alcohol than women who carried to term.(23) According to researcher Dr. Philip Ney, “If they are unable to legally obtain mood-altering drugs with a prescription, many of these women resort to alcohol or illegal drugs as a means of suppressing unwanted feelings about their past abortions.”(24)
Drug and alcohol abuse also put women at greater risk not only for violence, but for other self-destructive activities such as promiscuity (which can lead to repeat abortions, sexually-transmitted diseases and HIV/AIDS) and driving while intoxicated. Post-abortive women are also more likely to use drugs or alcohol during pregnancy,(25) which has been linked to brain damage in infants, premature delivery, miscarriage and a host of other problems. Those seeking a remedy for the current epidemic of drug and alcohol-addicted babies would do well to look at the role abortion is playing in this tragic problem.
Post-abortive women are also more likely to smoke than women with other pregnancy outcomes, which carries its own set of health risks.(26) For example, smoking during pregnancy has been associated with pregnancy loss, premature birth, low birth weight, Sudden Infant Death Syndrome, and neurological and respiratory problems in infants. Despite these risks, women with a history of abortion are more likely to smoke during subsequent pregnancies, perhaps a means of relieving post-abortion anxiety.(27)
The Mental Health Threat
Women with a history of abortion are more likely to experience depression than women who give birth, especially if they had negative feelings about the abortion or felt that they had no control over the abortion decision.(28) This is an important finding considering that our WEBA study of 252 post-abortive women found that more than 50 percent said they felt “forced” to abort by others or because of their circumstances.(29)
An Elliot Institute study of California women for up to six years after childbirth or abortion found that those who aborted had significantly higher mental health claims than women who carried to term.(30) And a Danish study found that overall, women with a history of abortion had a 50 percent higher rate of admission to psychiatric hospitals than did women who had live born children.(31)
Repeat abortion may be both a result and a trigger of emotional and psychological problems. A study of women seeking repeat abortions found a three-fold increase in previous psychiatric consultations compared with maternity patients who were carrying their children to term.(32)
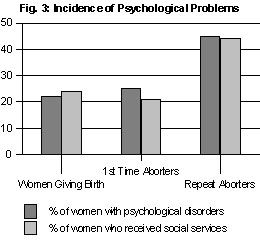 Another study (see Figure 3) found that while there was no significant difference in psychological disorders or use of social services between women carrying to term and those seeking abortion for the first time, women who had already had an abortion were almost twice as likely to have psychological disorders or to have had contact with the social service system.(33)
Another study (see Figure 3) found that while there was no significant difference in psychological disorders or use of social services between women carrying to term and those seeking abortion for the first time, women who had already had an abortion were almost twice as likely to have psychological disorders or to have had contact with the social service system.(33)
Conclusion
While it is important to educate women on abortion risks and promote post-abortion healing, we must do more. Women have a right to informed consent before abortion, a right that should be guaranteed by law. This right will only come, however, when laws protecting abortionists from liability are replaced by laws expanding women’s right to redress for physical and emotional injuries caused by abortion. Let us hope and pray that day comes soon.
Originally printed in The Post-Abortion Review, Issue 8(3), July-Sept. 2000. Copyright 2000, Elliot Institute.
Update: This article was initially published in 2000. For updated information about studies on the aftereffects of abortion, see here, here, here, here and here.
1. K. Sherlock, Victims of Choice (Arkon, OH: Brennyman Books, 1996) 134-135.
2. Kaunitz, “Causes of Maternal Mortality in the United States,” Obstetrics and Gynecology, 65(5), May 1985.
3. Gissler, M., et. al., “Pregnancy-associated deaths in Finland 1987-1994 – definition problems and benefits of record linkage,” Acta Obstetricia et Gynecolgica Scandinavica 76:651-657 (1997).
4. For a list of the known physical complications of abortion and citations to various studies, visit our web site at www.afterabortion.org.
5. T. Strahan, “Induced Abortion as a Contributing Factor in Maternal Mortality or Pregnancy-Related Death in Women,” Association for Interdisciplinary Research Bulletin, 10(3):3-4, Nov./Dec. 1996.
6. G. Niewsma,.”The Return of Do-It-Yourself Abortions,” Clarity, May/June 1994.
7. J.L. Sorenson et. al., “Early and Late Onset Pelvic Inflammatory Disease Among Women with Cervical Chlamydial Trachomatis Infection at the Time of Induced Abortion,” Infection, 22(4):242, 1994.
8. S.D. Hillis et. al., “Delayed care of pelvic inflammatory disease as a risk factor for impaired fertility,” Am. J. Obstet. and Gynecol., 168:1503-1509, 1993.
9. See T. Tburnakis and N. Hildebrandt, “Pelvic Inflammatory Disease: A Review With Emphasis on Antimicrobial Therapy,” Reviews of Infectious Diseases, 8(1):86, 1986; and J. Sorenson and I. Thronov, “A double-blind randomized study of erythromycin in preventing pelvic inflammatory disease after first-trimester abortion,” British J. Obstet. and Gynecol., 99:434, 1992.
10. The American Cancer Society, quoted in T. Strahan, “Childbirth as Protective of the Health of Women in Contrast to Induced Abortion. I. Breast, Ovarian, and Endometrial Cancer,” Research Bulletin, 12(2):1, Jan/Feb. 1998.
11. J. Brind et al., “Induced abortion as an independent risk factor for breast cancer: a comprehensive review and analysis,” J. of Epidemiology and Community Health, 50: 481-49.
12. B. E. Kwast, “The hypertensive disorders of pregnancy: their contribution to maternal mortality,” Midwifery, 7:157-161, 1991.
13. D. Campbell et al., “Pre-eclampsia in second pregnancy,” British Journal of Obstetrics and Gynaecology, 92:131-140, 1985.
14. C. Infante-Rivard and R. Gauthier, “Induced Abortion as a Risk Factor for Subsequent Fetal Loss,” Epidemiology, 7:540-542, 1986.
15. See A. Levin, et al., “Ectopic Pregnancy and Prior Induced Abortion,” Am J. Public Health, 72(3):253, March 1982; and A. Kalandidi, et al., “Induced Abortions, Contraceptive Practices, and Tobacco Smoking as Risk Factors for Ectopic Pregnancy in Athens, Greece,” British J. Obstet and Gynecol., 98:207-213, Feb. 1991.
16. M.A. Krohn, et. al., “Prior Pregnancy Outcome and the Risk of Intraamniotic Infection in the Following Pregnancy,” Am J. Obstet Gynecol, 178:381-385, 1998.
17. E.B. Obel, “Long-term sequelae following legally induced abortion,” Danish Med. Bull., 27:61, 1980.
18. G. Fridh et. al., “Factors Associated With More Intense Labor Pain,” Research in Nursing and Health, 11:117-124, 1988.
19. See M.H. Hall et al., “Concomitant and repeated happenings of complications of the third stage of labor,” British J Obstet Gynaecol, 92:732-738, July 1985; and A. Lopes, et. al., “The Impact of Multiple Induced Abortions on the Outcome of Subsequent Pregnancy,” Aust NZ J. Obstet Gynaecol., 31(1):41-43, 1991.
20. T. Strahan, “Induced Abortion as a Contribution Factor in Maternal Mortality or Pregnancy-Related Death in Women,” Assoc. for Interdisciplinary Research Bulletin, 10(3):7, Nov.-Dec. 1996.
21. D. Reardon, Aborted Women, Silent No More (Chicago, Loyola University Press, 1987), xviii.
22. R.F. Badgely et. al., Report of the Committee on Abortion Law, Supply and Services, Ottawa, 1977:313-321, as cited in L.L. De Veber et. al., “Postabortion Grief: Psychological Sequelae of Induced Abortion,” Humane Medicine, 7(3):203, Aug. 1991.
23. D. Reardon and P. Ney, “Abortion and Subsequent Substance Abuse,” The American Journal of Drug and Alcohol Abuse, 26(1):61-75, 2000.
24. “15th Study Links Abortion, Substance Abuse,” The Post-Abortion Review, 8(1):8, Jan.-March 2000.
25. See D.A. Frank, et. al., “Cocaine Use During Pregnancy: Prevalence and Correlates,” Pediatrics, 82(8):888, Dec. 1988; L.G. Keith, et. al., “Substance Abuse in Pregnant Women: Recent Experience at the Perinatal Center for Chemical Dependence of Northwestern Memorial Hospital,” Obstetrics & Gynecology, 73:715, 1989; and M. Plant, Women, Drinking and Pregnancy (London: Tavistock Publications, 1985).
26. See A. Lopes, et. al., “The Impact of Multiple Induced Abortions on the Outcome of Subsequent Pregnancy,” Australia New Zealand J. Obstet. Gynaecol., 31(1):41-43, 1991; S. Kullander and B. Kallen, “A Prospective Study of Smoking and Pregnancy,” Acta Obstet Gynecol Scandinavia, 50:83-94, 1971; C. J. Hogue, “Low birth weight subsequent to induced abortion. A historical prospective study of 948 women in Skopje, Yugoslavia,” American J. Obstet Gynecol, 123(7):678-681, Dec. 1, 1975.
27. M.T. Mandelson, C.B. Maden and J.R. Daling, “Low Birth Weight in Relation to Multiple Induced Abortions,” American J. Public Health, 82(3):391-394, March 1992.
28. C.F. Bradley, “Abortion and Subsequent Pregnancy Loss,” Canadian J. Psychiatry, 29:494-498, Oct. 1984.
29. G. Skelton, “Many in Survey Who Had Abortions Cite Guilt Feelings,” Los Angeles Times (March 19, 1989).
30. P. Coleman and D. Reardon, “State-Funded Abortions vs. Deliveries: A Comparison of Subsequent Mental Health Claims Over Six Years,” Poster presented at the 12th annual meeting of the American Psychological Society, Miami Beach, FL, June 2000.
31. H. David, N. Rasmussen and E. Holst, “Postpartum and Postabortion Psychotic Reactions,” Family Planning Perspectives, 13(2), March/April 1981, p. 8892.
32. W. Pasini. and J. Kellerhals, Proceedings of the Conference on Psycho-Social Factors in Transnational Family Planning Research (Washington, D.C.: American Institute for Research, 1970) 44-54.
33. Tornbom, M., et. al., “Repeat Abortion: A Comparative Study,” Journal of Psychosomatic Obstetrics and Gynecology, 17:208-214, 1996.

