Anticipating Abortion Risks to Mental Health
The decision to have an abortion can be difficult. The potential risks and benefits of abortion should be carefully evaluated. These risks will vary widely between different people and in different circumstances.
Unfortunately, as many as 62% of women thinking about abortion feel pressured by other people to undergo an abortion regardless of its risks.
So it is helpful to get decision making counseling from someone who is not biased in favor of an abortion. It can be helpful to talking with a well-informed counselor (preferably, by someone who is not employed by an abortion provider) to:
- better understand what you truly want and need,
- evaluate which of your options is most likely to satisfy your long term needs, and
- evaluate abortion’s risks and potential benefits relative to other options.
The chart below will help you consider the risks of abortion in light of your own unique personality and situation. It is also important to share these risks with anyone who might be encouraging you to choose an abortion.
Finally, it is important to know that there is no evidence that abortion ever contributes to improved mental health. To the contrary, reviews of all the published studies compare abortion to carrying an unplanned pregnancy to term indicate that there is an increase, not a decrease, in mental health issues.
RISK FACTORS PSYCHOLOGICAL AND EMOTIONAL COMPLICATIONS
The American Psychological Association’s task force on abortion and mental health reports that the following risk factors predict who will have the most problems after an abortion:1–6
You are at greater risk if you:
- already have a prior history of abortion
- are younger than 20 years of age
- have a history of any mental health problems
- are feeling any pressure from others to have an abortion
- feel the decision to abort is not your own or is your only choice
- previously wanted or planned to become pregnant
- have a strong maternal orientation or already have children
- are having an abortion because of known or suspected fetal malformation
- are feeling some emotional attachment to this pregnancy or baby
- believe, or were raised to believe, abortion is morally wrong
- feel there is a stigma attached to abortion
- feel a need to keep your abortion secret
- have been exposed to antiabortion picketing
- feel ambivalent or uncertain about having an abortion or carrying to term
- feel like you’re going to have trouble coping with an abortion
- have low self-esteem, a pessimistic outlook, low perceived control over your life or other personality traits that may limit your coping skills
- tend to cope with unpleasant thoughts is through repression, denial, or substance use
- feel a lack of support to have the abortion from significant others
- lack of support to keep the baby from significant others
- feel or expect opposition from significant others to having an abortion
- are having an abortion after 12 weeks gestation
- are having an abortion because of health reasons (to preserve your physical health)
This is only a partial list of all known the known abortion risk factors.2,3 But it is a good start.
It is highly recommended that can review this checklist with your doctor. Your doctor should evaluate the risks versus the benefits of you having an abortion in light of these risk factors. Any doctor who ignores these risk factors is guilty of negligent pre-abortion screening.
Make sure to discuss these abortion risk factors with a doctor before having an abortion.
NEGATIVE EMOTIONS AND MENTAL HEALTH RISKS AFTER AN ABORTION
Abortion can both relieve stress and create stress.1 Negative feelings are common before and after an abortion. Some women may feel mostly just relief after an abortion. But it is more common for women to have a mix of feelings, including positive feelings and negative feelings.7–13 More women report negative feelings than positive ones.6
Negative feelings may appear immediately or much later. Many women report feeling fine in the first days and weeks after an abortion with negative emerging only much later. These delayed reactions are often triggered by some other experience. For example, a subsequent pregnancy, a miscarriage, the birth of child, a death in the family, or a religious conversion.14,15 In general, positive emotions decrease with time while negative emotions increase.6,8
Not all negative feelings after an abortion rise to the level of being a mental illness.1 But no matter what the level of severity of negative reactions, counseling may help.
It is unclear when, if ever, abortion is the sole cause of mental health problems. But there is no doubt that abortion contributes to mental health problems. At the very least, it can trigger, complicate or worsen pre-existing psychological problems.1,6,16
Abortion is statistically linked to elevated risks of suicide attempts16–19 and completed suicide,20–22 sleep disorders,23 addiction or misuse of drugs and/or alcohol,16,18,24–28 bi-polar disorder,29–31 depression,1,16,31–36 anxiety,16,25,27,28,31,36 posttraumatic stress disorder, 8,9,13,37–50 anger or rage,14 difficulties parenting,51–53 increased risk of premature death,54–56 and other emotional or mental health issues.14
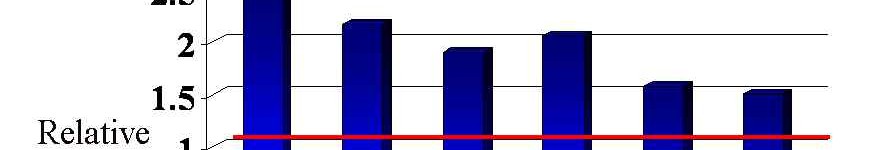
The chart above shows the percent of increased risk various mental health problems following abortion as measured in selected studies.
The length of the line shows the statistical range in which the “true” increased risk is most likely to lie. (The numbers in parenthesis at the right show this range precisely.) For example, the study examining sleep disorders found that women who had abortions were 68% more likely to require treatment for a sleep disorder in the year following an abortion. But the line shows a range from 18% to 140%. This means that given the size of the study, there is a 95% chance that similar studies would find results between 18% and 140%. This range is called the 95% confidence interval. As you can see, in most cases, even the lowest number in that range indicated a higher risk of that symptom after an abortion.
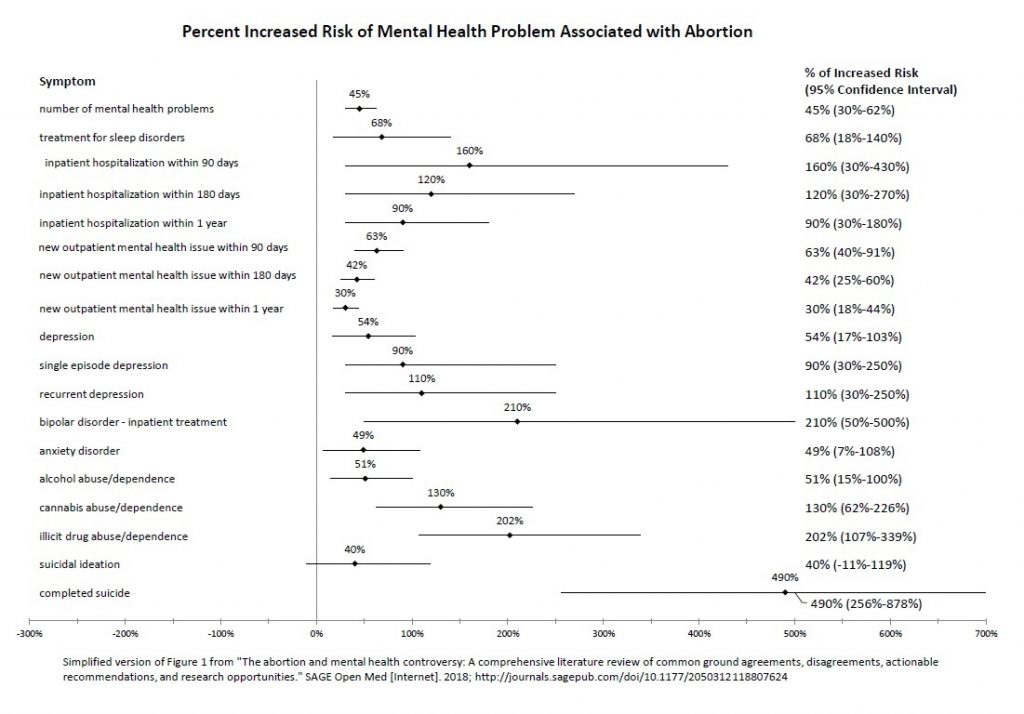
Another way of looking at the mental health risks of abortion is to look at the percentage of specific mental health problems that may be attributable to abortion. The chart below is based on a survey of a nationally representative sample of women funded by the federal government.16
This chart shows a statistic called the “population attributable fraction,” or PAF, for various psychological problems that are statistically attributable abortion.16 The numbers in parenthesis show the statistical range in which the “true” PAF is 95% most likely to lie.
For example, the finding for depression indicates that 10.7 percent of all cases of substance use disorders may be due to abortion. The confidence interval, however, indicates that the “true” number is most likely somewhere between 6.9 and 14.4 percent of all cases of substance use disorders.
SYMPTOMS OF STRESS AFTER AN ABORTION
While abortion stress may contribute to mental illness, it is more likely to show up as just negative feelings.14 Some common feelings are:
- Sadness
- Loss or emptiness
- Anger and a shorter fuse
- Jealously or aversion to pregnant women or babies
- Fear of a doctor’s office or other place that reminds you of the abortion
- Shame, guilt, self-blame
- Distanced, or alienation from others
- A “before” and “after” feeling; you are a different person after the abortion
- Overprotectiveness of your children
- Viewing a miscarriage or infertility problems as a “punishment”
- Heightened fear of making wrong decisions
Many women experience more problems in their relationships following an abortion.14 This can include:
- fear of being judged by one’s partner
- more problems with sex
- heightened fear of pregnancy (and another abortion)
- less pleasure with sex
- more conflict with anyone involved in the abortion decision
- compelling anxiety for a replacement pregnancy
- withdrawal and isolation from previous relationships
- new fears regarding emotional or sexual intimacy
“Connectors,” like the following, may subconsciously trigger unresolved feelings about a prior abortion: 14
- seeing babies or pregnant women
- vacuum sounds similar to the abortion machine
- doctor’s offices
- the street where the abortion clinic was
- a smell or food you link to a something you at the day of the abortion
- an anniversary reaction: the time of the year of the abortion or the expected due date
More severe reactions can include the start or worsening of: 14
- Depression
- Self-blame, self-hate, self-sabotage
- Suicidal thoughts or self-harm
- More drinking or drug use (self-medication)
- Numbing out (deadening of emotions)
- Flashbacks, involuntary thoughts
- Nightmares
- Sleeping difficulties
- Anxiety attacks or startle reactions
- Eating disorders
- Emotional distancing from your children or spouse
- Compulsions, such as a need to look at pictures of developing fetuses, even though it hurts rather than helps
The Abortion and Mental Health Controversy
Like any topic touching on abortion, the effects of abortion on mental health have been drawn into this political conflict. Abortion defenders often claim that the American Psychological Association (APA) and other experts have proven that abortion does not have any mental health risks.6 This is simply not true.
The APA committed itself to a political position in favor of a woman’s right to abortion way back in 1969. Their support for abortion is admittedly based on a political view, not on any evidence that abortion improves mental health. As a result, the APA’s reports on abortion have definite political “spin” that de-emphasizes the risks of abortion. But when you read their reports carefully, you will see that they actually agree that abortion can contribute to mental health problems.6 What they are denying is only that there is sufficient evidence to be certain that abortion is ever the sole cause of mental health problems.6
The APA does not dispute the undeniable fact that women with a history of abortion have higher rates of mental illness compared to other groups of women.6 The controversy is over how to explain this fact.
As noted in the list of risk factors at the top of this article, a history of prior mental illness is a risk factor for more problems after an abortion. Understandably, women with a prior history of depression are also more likely to report depression after an abortion. Abortion is never a cure for mental health problems, but it can contribute to a worsening of those problems.
This is the crux of the controversy between abortion advocates and abortion critics.
Abortion advocates are trying to minimize the link between abortion and mental health risks. They are arguing that prior tendencies toward mental illness are full explanation for the higher rates of mental illness after an abortion. Most pro-choice experts will admit that abortion may aggravate or complicate these prior tendencies toward mental illness, but it their chief argument that abortion is not the sole cause, in and of itself, of the elevated risks of mental illness seen in national samples.6
Are women with prior mental health problems more likely to be further disturbed by an abortion? Of course. Does this finding prove that mentally healthy women are never disturbed by an abortion? Of course not.
The question of causation is an important one. But it most cases, there are multiple factors of causation, not a single factor.
In any event, even if the APA’s claim that abortion is not the sole cause of mental illnesses is true, the fact that abortion is marker for increased need of mental health services is still true, too.
The bottom line: women with a history of abortion are at greater risk of the emotional problems outlined above. Therefore, access to post-abortion support and counseling is important to women’s health.
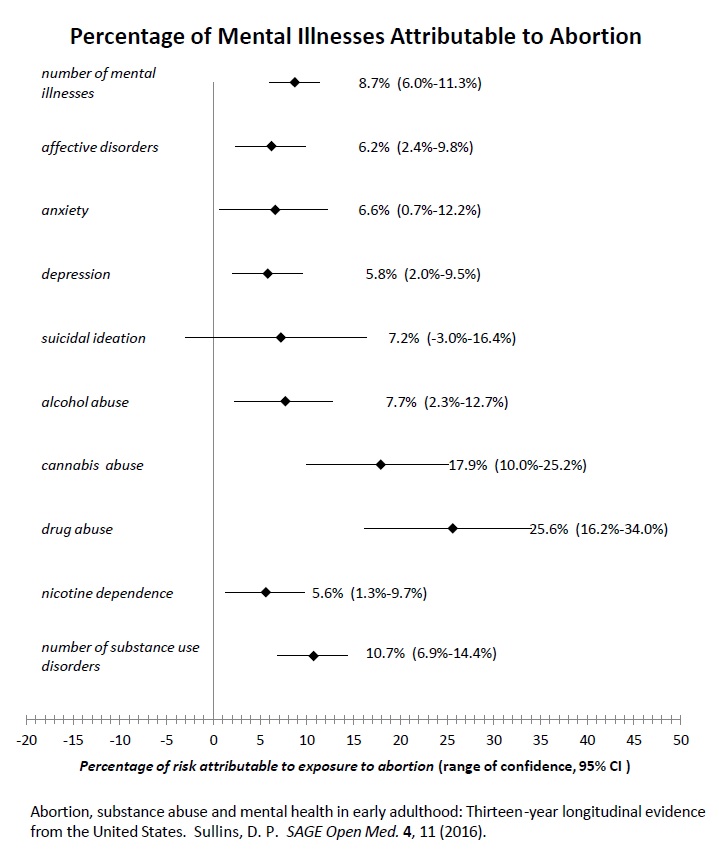
Rate of psychiatric hospitalization after abortion compared to childbirth
PHYSICAL COMPLICATIONS AFTER AN ABORTION
Abortion’s risks include negative impacts on women’s general health, especially their future reproductive health, and longevity. Please read this related article focused on the complications of abortion related to physical health.
Related Articles
- Abortion Contributes to Mental Health Problems: Both Sides Agree According to a Comprehensive Medical Review
- Abortion and Mental Health Risks: A Closer Look
- Ad Hominem Attacks, Guilt by Association, Shifting Standards, Avoiding Simple Truths
- “Evidence Doesn’t Matter,” APA Spokesperson Says of Abortion Complications
References
1. Major, B. et al. Report of the APA Task Force on Mental Health and Abortion. (American Psychological Association, 2008).
2. Reardon, D. C. Abortion decisions and the duty to screen: clinical, ethical, and legal implications of predictive risk factors of post-abortion maladjustment. J. Contemp. Health Law Policy 20, 33–114 (2003).
3. Coleman, P. K. Women at risk for post-abortion mental health problems and abortion associated relationship challenges. in Post-abortion Trauma: Possible Psychological and Existential Aftermaths 147–210 (Pontifical Academy for Life, 2014).
4. Baker, A. & Beresford, T. Informed consent, patient education and counseling. in Management of Unintended and Abnormal Pregnancy: Comprehensive Abortion Care (eds. Paul, M. et al.) (Wiley-Blackwell, 2009).
5. Shuping, M. Risk Factors. in Peace Psychology Perspectives on Abortion (ed. MacNair, R. M.) (Feminism {&} Nonviolence Studies Association, 2016).
6. Reardon, D. C. The abortion and mental health controversy: A comprehensive literature review of common ground agreements, disagreements, actionable recommendations, and research opportunities. SAGE Open Med. 6, 205031211880762 (2018).
7. Miller, W. An empirical study of the psychological antecedents and consequences of induced abortion. J. Soc. Issues 48, 67–93 (1992).
8. Major, B. et al. Psychological responses of women after first-trimester abortion. Arch. Gen. Psychiatry 57, 777–784 (2000).
9. Rue, V. M., Coleman, P. K., Rue, J. J. & Reardon, D. C. Induced abortion and traumatic stress: A preliminary comparison of American and Russian women. Med. Sci. Monit. 10, SR5–SR16 (2004).
10. Kero, A. & Lalos, A. Ambivalence–a logical response to legal abortion: a prospective study among women and men. J. Psychosom. Obstet. Gynaecol. 21, 81–91 (2000).
11. Söderberg, H., Janzon, L. & Sjöberg, N. O. Emotional distress following induced abortion: a study of its incidence and determinants among abortees in Malmö, Sweden. Eur. J. Obstet. Gynecol. Reprod. Biol. 79, 173–8 (1998).
12. Zimmerman, M. K. Passage Through Abortion: The Personal and Social Reality of Women’s Experiences. (Praeger Publishers, 1977).
13. Suliman, S. et al. Comparison of pain, cortisol levels, and psychological distress in women undergoing surgical termination of pregnancy under local anaesthesia versus intravenous sedation. BMC Psychiatry 7, 24 (2007).
14. Burke, T. & Reardon, D. C. Forbidden Grief: The Unspoken Pain of Abortion. (Acorn Books, 2007).
15. Stotland, N. L. Psychiatric aspects of induced abortion. Arch. Womens. Ment. Health 4, 27–31 (2001).
16. Sullins, D. P. Abortion, substance abuse and mental health in early adulthood: Thirteen-year longitudinal evidence from the United States. SAGE Open Med. 4, 11 (2016).
17. Morgan, C. L., Evans, M. & Peters, J. R. Suicides after pregnancy. Mental health may deteriorate as a direct effect of induced abortion. BMJ 314, 902 (1997).
18. Fergusson, D. M., Horwood, L. J. & Boden, J. M. Does abortion reduce the mental health risks of unwanted or unintended pregnancy? A re-appraisal of the evidence. Aust. N. Z. J. Psychiatry 47, 819–27 (2013).
19. Luo, M. et al. Association between induced abortion and suicidal ideation among unmarried female migrant workers in three metropolitan cities in China: a cross-sectional study. BMC Public Health 18, 625 (2018).
20. Gissler, M., Hemminki, E., Lönnqvist, J. & Lonnqvist, J. Suicides after pregnancy in Finland, 1987-94: register linkage study. BMJ 313, 1431–1434 (1996).
21. Reardon, D. C. et al. Deaths associated with pregnancy outcome: A record linkage study of low income women. South. Med. J. 95, 834–841 (2002).
22. Appleby, L. Suicide during pregnancy and in the first postnatal year. Br. Med. J. 302, 137–140 (1991).
23. Reardon, D. C. & Coleman, P. K. Relative treatment rates for sleep disorders and sleep disturbances following abortion and childbirth: a prospective record-based study. Sleep 29, 105–106 (2006).
24. Coleman, P. K., Reardon, D. C., Rue, V. M. & Cougle, J. A history of induced abortion in relation to substance abuse during subsequent pregnancies carried to term. Am. J. Obstet. Gynecol. 187, 1673–8 (2002).
25. Dingle, K., Alati, R., Clavarino, A., Najman, J. M. & Williams, G. M. Pregnancy loss and psychiatric disorders in young women: An Australian birth cohort study. Br. J. Psychiatry 193, 455–460 (2008).
26. Pedersen, W. Childbirth, abortion and subsequent substance use in young women: A population-based longitudinal study. Addiction 102, 1971–1978 (2007).
27. Fergusson, D. M., Horwood, L. J. & Boden, J. M. Abortion and mental health disorders: Evidence from a 30-year longitudinal study. Br. J. Psychiatry 193, 444–451 (2008).
28. van Ditzhuijzen, J. et al. Incidence and recurrence of common mental disorders after abortion: Results from a prospective cohort study. J. Psychiatr. Res. 84, 200–206 (2017).
29. Marengo, E. et al. Unplanned pregnancies and reproductive health among women with bipolar disorder. J. Affect. Disord. 178, 201–205 (2015).
30. Coleman, P. K., Reardon, D. C., Rue, V. M. & Cougle, J. State-funded abortions versus deliveries: a comparison of outpatient mental health claims over 4 years. Am. J. Orthopsychiatry 72, 141–52 (2002).
31. Reardon, D. C. et al. Psychiatric admissions of low-income women following abortion and childbirth. CMAJ 168, 1253–1256 (2003).
32. Cougle, J. R., Reardon, D. C. & Coleman, P. K. Depression associated with abortion and childbirth: a long-term analysis of the NLSY cohort. Med. Sci. Monit. 9, CR105-R112 (2003).
33. Pedersen, W. Abortion and depression: a population-based longitudinal study of young women. Scand. J. Public Health 36, 424–428 (2008).
34. Steinberg, J. R., Laursen, T. M., Adler, N. E. & Gasse, C. Examining the Association of Antidepressant Prescriptions With First Abortion and First Childbirth. JAMA Psychiatry 20742, 1–7 (2018).
35. Meltzer-Brody, S. et al. Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol. Med. 1–15 (2017). doi:10.1017/S0033291716003020
36. Gong, X. et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. Eur. J. Obstet. Gynecol. Reprod. Biol. 166, 30–6 (2013).
37. Coleman, P. K., Coyle, C. T. & Rue, V. M. Late-term elective abortion and susceptibility to posttraumatic stress symptoms. J. Pregnancy 2010, 130519 (2010).
38. Hamama, L., Rauch, S. a M., Sperlich, M., Defever, E. & Seng, J. S. Previous experience of spontaneous or elective abortion and risk for posttraumatic stress and depression during subsequent pregnancy. Depress. Anxiety 27, 699–707 (2010).
39. Kersting, A. et al. Psychological impact on women after second and third trimester termination of pregnancy due to fetal anomalies versus women after preterm birth-a 14-month follow up study. Arch. Womens. Ment. Health 12, 193–201 (2009).
40. Kelly, T., Suddes, J., Howel, D., Hewison, J. & Robson, S. Comparing medical versus surgical termination of pregnancy at 13-20weeks of gestation: A randomised controlled trial. BJOG An Int. J. Obstet. Gynaecol. 117, 1512–1520 (2010).
41. Borins, E. F. M. & Forsythe, P. J. Past trauma and present functioning of patients attending a women’s psychiatric clinic. Am. J. Psychiatry 142, 460–463 (1985).
42. Fisch, R. Z. & Tadmor, O. Iatrogenic post-traumatic stress disorder. Lancet (London, England) 2, 1397 (1989).
43. Vukelić, J., Kapamadzija, A. & Kondić, B. [Investigation of risk factors for acute stress reaction following induced abortion]. Med. Pregl. 63, 399–403
44. Giannandrea, S. A. M., Cerulli, C., Anson, E. & Chaudron, L. H. Increased risk for postpartum psychiatric disorders among women with past pregnancy loss. J. Womens. Health (Larchmt). 22, 760–8 (2013).
45. Wallin Lundell, I. et al. Neuroticism-related personality traits are associated with posttraumatic stress after abortion: findings from a Swedish multi-center cohort study. BMC Womens. Health 17, 96 (2017).
46. Daugirdaitė, V., van den Akker, O. & Purewal, S. Posttraumatic Stress and Posttraumatic Stress Disorder after Termination of Pregnancy and Reproductive Loss: A Systematic Review. J. Pregnancy 2015, 1–14 (2015).
47. Montmasson, H., Bertrand, P., Perrotin, F. & El-Hage, W. Facteurs prédictifs de l’état de stress post-traumatique du postpartum chez la primipare. J. Gynécologie Obs. Biol. la Reprod. 41, 553–560 (2012).
48. Zulčić-Nakić, V., Pajević, I., Hasanović, M., Pavlović, S. & Ljuca, D. Psychological problems sequalae in adolescents after artificial abortion. J. Pediatr. Adolesc. Gynecol. 25, 241–7 (2012).
49. Rousset, C., Brulfert, C., Séjourné, N., Goutaudier, N. & Chabrol, H. Posttraumatic Stress Disorder and psychological distress following medical and surgical abortion. J. Reprod. Infant Psychol. 29, 506–517 (2011).
50. Van Rooyenm, M. & Smith, S. The prevalence of post-abortion syndrome in patients presenting at Kalafong hospital ’ s family medicine clinic after having a termination of pregnancy. SA Fam Pr. 46, 21–24 (2004).
51. Coleman, P. The Psychological Pain of Perinatal Loss and Subsequent Parenting Risks: Could Induced Abortion be more Problematic than Other Forms of Loss. Curr. Womens. Health Rev. 5, 88–99 (2009).
52. Coleman, P. K., Reardon, D. C. & Cougle, J. The quality of the caregiving environment and child development outcomes associated with maternal history of abortion using the NLSY data. J. Child Psychol. Psychiatry Allied Discip. 43, 743–757 (2002).
53. Coleman, P. K., Maxey, C. D., Spence, M. & Nixon, C. L. Predictors and correlates of abortion in the fragile families and well-being study: Paternal behavior, substance use, and partner violence. Int. J. Ment. Health Addict. 7, 405–422 (2009).
54. Gissler, M., Berg, C., Bouvier-Colle, M.-H. & Buekens, P. Pregnancy-associated mortality after birth, spontaneous abortion, or induced abortion in Finland, 1987-2000. Am. J. Obstet. Gynecol. 190, 422–7 (2004).
55. Reardon, D. C., Strahan, T. W., Thorp, J. M. & Shuping, M. W. Deaths associated with abortion compared to childbirth–a review of new and old data and the medical and legal implications. J. Contemp. Health Law Policy 20, 279–327 (2004).
56. Coleman, P. K., Reardon, D. C. & Calhoun, B. C. Reproductive history patterns and long-term mortality rates: A Danish, population-based record linkage study. Eur. J. Public Health 23, 569–574 (2013).